BROOMFIELD, Colo. — On the bike, three‑time Ironman World Championship competitor Kristin Jenny is used to racing the clock. But in August, she received a different kind of challenge.
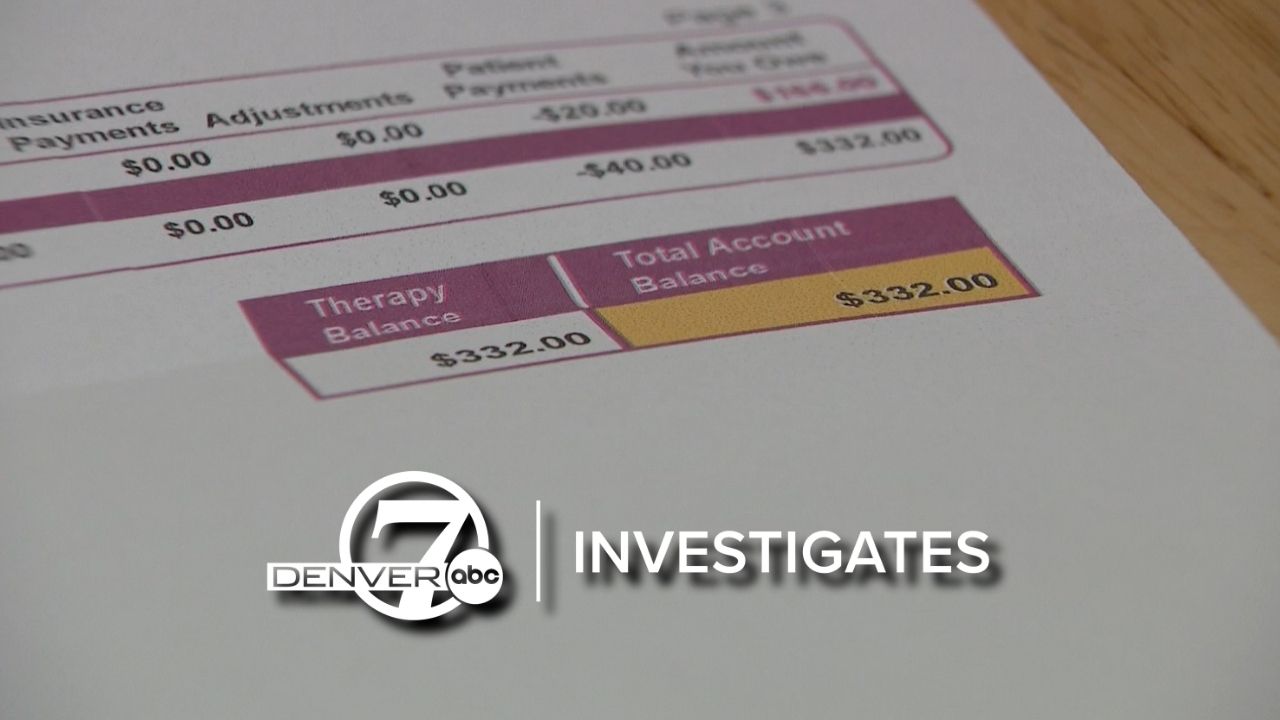
Jenny received a $332 bill from Boulder Community Health for two physical therapy appointments she had in March 2022 — appointments she thought her insurance had already paid.
“The bill is due Sept. 27, 2025,” she told Denver7 Investigates. “A bill for anything three-and-a-half years later is shocking to me."

Jenny had knee surgery in 2021 and was referred to CU Sports Medicine, which bills through Boulder Community Health, for physical therapy.
“My understanding at the time was, pay the $20 copay and be on my way,” she said. “I saw this physical therapy provider about 10 times. I’m a little freaked out that I’m actually going to ultimately owe thousands of dollars."
When Boulder Community Health told her the claim had been "re-run," she called her former insurer, Horizon Blue Cross Blue Shield of New Jersey, and was told her former account would need to be "unarchived."
“I called back just a couple of days ago and actually had to start the whole process again," Jenny said. "They didn’t seem to have done anything, and that’s when I reached out to you."
"No patient should be receiving a bill years after the fact."
Colorado law allows health care providers to bill patients up to six years after receiving services.
Adam Fox, deputy director at the Colorado Consumer Health Initiative, said that may be legal, but he believes it’s not how the health care system should function.
“No patient should be receiving a bill years after the fact and be expected to pay it,” Fox said. “I think when we have seen these late bills, it tends to feel predatory and extractive. It makes it nearly impossible for the patient or consumer to have that covered by their insurance or fight the bill. I think, ideally, we need to set realistic timelines for healthcare billing."
Provider’s explanation
In a statement, Boulder Community Health said the claim was originally processed by Anthem Blue Cross Blue Shield (BCBS) in 2022 as a covered service, but Anthem BCBS reprocessed the claim and "reclassified the service as non-covered under the patient's plan."
“The claim in question was originally processed by Anthem Blue Cross Blue Shield (Anthem BCBS) in 2022 as a covered service. BCH recently received a new remittance from Anthem BCBS indicating that they reprocessed the claim and reclassified the service as non-covered under the patient’s plan. By law, health care providers are required to adhere to the information provided by an insurer in their remittance notices. We have reached out to Anthem BCBS to understand the reason for this reprocessing and to verify the accuracy of their updated claim classification. While we continue our review and communication with Anthem BCBS, we will place any related patient statements on hold.”
Anthem BCBS has not yet responded to Denver7 Investigates' request for comment. However, in an email to Jenny, a representative said they were reviewing the claim after Denver7 Investigates reached out.
“Now it says pending insurance and that my current balance is $0,” Jenny said.
Though the bill is currently on hold, Jenny called the process to dispute it exhausting.
“I’m someone who usually can resolve things on my own, so I appreciate the work you’re doing, but I don’t love that I had to escalate it this far," she said.